Why I Don’t Use Hip Bone for Neck Fusion
 Summary:
Summary:- Hip pain can be as bad as the neck surgery
- Rarely would hip bone need to be used
- Studies show in most cases hip bone on advantage
 Why we don’t use hip (iliac crest) bone for fusing the cervical spine
Why we don’t use hip (iliac crest) bone for fusing the cervical spine
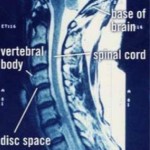
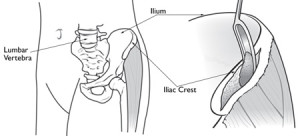
A persons hip bone or iliac crest bone is still commonly used by some surgeons as graft bone to be placed in the disc space following anterior cervical discectomy and fusion (ACDF) surgery. The use of this bone graft as a spacer following ACDF is often used along with a plate in order to hold the spine stable as the bone fusion takes place. Advancements in this plate technology as well as our ability to prepare donor bone for fusion implantation has allowed many surgeons to avoid taking the hip bone for use as a graft. Using donor bone with or without cervical plates has resulted in similar fusion results with our patients and we thereby have avoided the problems and pain associated with acquiring the hip bone at the time of surgery.
These advances and other factors regarding your surgery and what type of implants will be used will be discussed with you by your neurosurgeon prior to surgery. Listed below is abstract or a summary of an article written by Jeff S. Silber, MD, etal, which relates his findings of long term hip pain which may occur after the hip bone is taken for ACDF surgery. There are many scientific articles that are written regarding this issue and your neurosurgeon can help answer any question you may have. This abstract findings along with other articles and the many years of experience of our neurosurgeons operating on thousands of patients has led us to our current standard of practice which is not to take the hip bone. Each patient, however, will have their own individual needs and requirements if surgery is indicated and therefore we treat every patient individually.
Donor Site Morbidity After Anterior Iliac Crest Bone Harvest for Single-Level Anterior Cervical Discectomy and Fusion
Jeff S. Silber, MD; D. Greg Anderson, MD ; Scott D. Daffner, MD ; Brian T. Brislin, MD ; J. Martin Leland, BA ; Alan S. Hilibrand, MD ; Alexander R. Vaccaro, MD ; Todd J. Albert, MD 2003; 28(2):134-139,
Study Design
This retrospective, questionnaire-based investigation evaluated iliac crest bone graft (ICBG) site morbidity in patients having undergone a single-level anterior cervical discectomy and fusion (ACDF) procedure performed by a single surgeon (T.J.A.).
Objective
To evaluate acute and chronic problems associated with anterior ICBG donation, particularly long-term functional outcomes and impairments caused by graft donation.
Summary of Background Data.
Anterior cervical discectomy and fusion procedures frequently use autologous anterior ICBG to facilitate osseous union. Although autologous ICBG offers several advantages over alternative grafting materials, donor site morbidity can be significant. Acute and chronic complications of donor sites have been reported, yet there are currently no reports of long-term functional outcomes after autologous anterior ICBG donation after single-level ACDF.
Methods
A questionnaire was mailed to 187 consecutive patients who were retrospectively identified to have undergone autologous anterior ICBG harvest for single-level ACDF between 1994 and 1998. The questionnaire divided items into symptomatic (acute and chronic) and functional assessments. Patients answered yes, no, or not applicable; pain was assessed with a Visual Analogue Scale (VAS).
Results
Surveys were completed either by mail or follow-up telephone interview by 134 patients (71.6%). Average follow-up was 48 months (range, 24-72 months). Acute symptoms were reported at the following rates: ambulation difficulty, 50.7%; extended antibiotic usage, 7.5%; persistent drainage, 3.7%; wound dehiscence, 2.2%; and incision and drainage, 1.5%. The chronic symptom questionnaire demonstrated a high degree of satisfaction with the cosmetic result (92.5%). Pain at the donor site was reported by 26.1% of patients with a mean VAS score of 3.8 in 10, and 11.2% chronically use pain medication. Twenty-one patients (15.7%) reported abnormal sensations at the donor site, but only 5.2% reported discomfort with clothing. A unique functional assessment revealed current impairments at the following rates: ambulation, 12.7%; recreational activities, 11.9%; work activities, 9.7%; activities of daily living, 8.2%; sexual activity, 7.5%; and household chores, 6.7%.
Conclusions
A large percentage of patients report chronic donor site pain after anterior ICBG donation, even when only a single-level ACDF procedure is performed. Moreover, long-term functional impairment can also be significant. Patients should be counseled regarding these potential problems, and alternative sources of graft material should be considered.
Tri-State Neurosurgical Associates-UPMC
Administrative Oakland Office Address:
Presbyterian University Hospital
Department of Neurosurgery
Suite 5C
200 Lothrop Street
Pittsburgh, PA 15213
Phone: 1-888-234-4357
© 2013 Tri-State Neurosurgical Associates – UPMC


 Dr. Maroon received an athletic scholarship to Indiana University in Bloomington, Indiana where as an undergraduate, he was named a Scholastic All-American in football. Dr. Maroon has successfully maintained his personal athletic interests through participation in 9 marathons and more than 72 Olympic-distance triathlon events. However, his greatest athletic accomplishment is his participation in 8 Ironman triathlons (Hawaii – 1993, 2003, 2008, 2010, 2013; Canada – 1995; New Zealand – 1997; Germany – 2000), where he usually finishes in the top 10 of his age group. Recently, in July 2012 and 2013, he finished second and third, respectively, in his age group in the Muncie, Indiana half Ironman triathlon. In October 2013 he completed his 5th World Championship Ironman in Kona, Hawaii.
Dr. Maroon received an athletic scholarship to Indiana University in Bloomington, Indiana where as an undergraduate, he was named a Scholastic All-American in football. Dr. Maroon has successfully maintained his personal athletic interests through participation in 9 marathons and more than 72 Olympic-distance triathlon events. However, his greatest athletic accomplishment is his participation in 8 Ironman triathlons (Hawaii – 1993, 2003, 2008, 2010, 2013; Canada – 1995; New Zealand – 1997; Germany – 2000), where he usually finishes in the top 10 of his age group. Recently, in July 2012 and 2013, he finished second and third, respectively, in his age group in the Muncie, Indiana half Ironman triathlon. In October 2013 he completed his 5th World Championship Ironman in Kona, Hawaii.