Understanding Concussion Beyond the Media Headlines
There are an estimated 1.6-3.8 million sports and recreation related concussions each year in the United States. Of these the vast majority occur in youths ≤ 19 years old, mostly male. Of the millions of concussion only about 200,000 are evaluated in the emergency room (ED). Motor vehicles, falls and bicycle injuries are still the greatest causes of TBIs in youths, but in organized sports wrestling, football, ice hockey, lacrosse and girls soccer have the greatest incidences of concussion. Greater than 15% of all high school sports related injuries are due to concussions.
There have been significant rule, equipment and concussion management changes to address this problem. Despite this there remains calls for an outright ban of youth football. Despite a particularly one sided debate which highlights potential negative consequences, athletes from youth to professional levels continue to enjoy participating and competing in football, and benefit from the numerous health, educational and leadership opportunities associated with this sport.
The Washington Times Editorial by Drs Joseph Maroon and Julian Bailes
 In January 2015 The Washington Times newspaper published an op ed letter by neurosurgeons Dr Joseph Maroon and Dr. Julian Bailes, entitled – Weighing the childhood risks of contact sports -Staying on the sidelines carries far more health danger than getting into the game. In this letter Drs. Maroon and Bailes discuss how a more balanced discussion is needed when understanding the actual risk and occurrence of sports-related concussion especially in youth football. As they point out today’s organized youth football leagues have evolved and use safety standards that were unheard of 10 or 20 years ago. Read online article HERE
In January 2015 The Washington Times newspaper published an op ed letter by neurosurgeons Dr Joseph Maroon and Dr. Julian Bailes, entitled – Weighing the childhood risks of contact sports -Staying on the sidelines carries far more health danger than getting into the game. In this letter Drs. Maroon and Bailes discuss how a more balanced discussion is needed when understanding the actual risk and occurrence of sports-related concussion especially in youth football. As they point out today’s organized youth football leagues have evolved and use safety standards that were unheard of 10 or 20 years ago. Read online article HERE
The incidence and severity of brain injury is one of the hottest topics in sports media today, and it is creating a storm of near-panic in youth sports — especially football. We worry that the public’s misunderstanding of the available medical research is the gravest threat facing organized contact sport at the youth and high school levels.
Understanding Athletic Concussion and CTE: What are the Risks?
 When an athlete, whether it is football, soccer, lacrosse or any sport, suffers a blow to head depending on the force, direction and condition of the athlete a concussion can occur. It can be painful for the athlete as well as frightening to a spectator to watch. We instinctively know we must protect our brain from trauma. Our hands reflexively move to our head to block an incoming blow.Over the last several years concussion researchers and the medical community have reported definitive evidence that a brain concussion can have both short-term and long-term negative consequences and must be treated properly just like any other injury. Despite this media stories continue to report on athletes, from pee-wee leagues through the pros, who are ignoring these warning and lying about having suffered a concussion.Research being done on those that suffered a concussion, both living and deceased, continues to indicate that blows to the head can have consequences to both brain function and structure. Like all other organs and parts of the body the consequences of abuse will eventually be revealed as we age. A knee joint traumatized daily in sport with running, stopping, twisting and being hit will eventually develop stiffness, soreness, swelling and degenerative changes leading to some type of disability. The brain may also suffer in this same way as a result of trauma and just as the knee this is most likely in part due to our own body’s inflammatory response. Prevention and proper initial management are essential.
When an athlete, whether it is football, soccer, lacrosse or any sport, suffers a blow to head depending on the force, direction and condition of the athlete a concussion can occur. It can be painful for the athlete as well as frightening to a spectator to watch. We instinctively know we must protect our brain from trauma. Our hands reflexively move to our head to block an incoming blow.Over the last several years concussion researchers and the medical community have reported definitive evidence that a brain concussion can have both short-term and long-term negative consequences and must be treated properly just like any other injury. Despite this media stories continue to report on athletes, from pee-wee leagues through the pros, who are ignoring these warning and lying about having suffered a concussion.Research being done on those that suffered a concussion, both living and deceased, continues to indicate that blows to the head can have consequences to both brain function and structure. Like all other organs and parts of the body the consequences of abuse will eventually be revealed as we age. A knee joint traumatized daily in sport with running, stopping, twisting and being hit will eventually develop stiffness, soreness, swelling and degenerative changes leading to some type of disability. The brain may also suffer in this same way as a result of trauma and just as the knee this is most likely in part due to our own body’s inflammatory response. Prevention and proper initial management are essential.
 Chronic progressive traumatic encephalopathy or CTE
Chronic progressive traumatic encephalopathy or CTE
Since the late 1920’s scientist have recognized head trauma can induce neurodegeneration when examined during an autopsy. First described as “Punch drunk syndrome” in boxers, later called dementia pugilistica (DP), and then more recently chronic progressive traumatic encephalopathy or CTE this condition has become a major health concern in amateur and professional sports. Currently, there are no definitive tests to distinguish CTE from other neurodegenerative diseases other than by evaluation of brain tissue. For this reason published reports of CTE thus far have been limited to individual and small collections of case studies of mostly former athletes who had a history of dementia of major psychological issues.
CTE has now been reported in a wide range of individual athletes, combat military personnel and others who had suffered some form of traumatic brain injury (TBI) years to decades prior to their deaths. Because concussions and blows to the head are common in both sports and the military there is a concern by many former athletes and veterans that symptoms of dementia and other brain related problems, especially with aging, may have some relationship to prior head trauma.
Brain Degeneration: CTE vs Alzheimer’s Disease
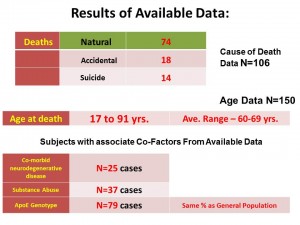
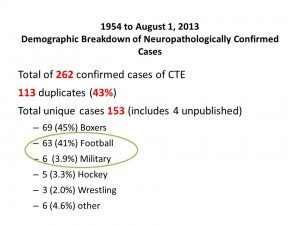 Because of these concerns an enormous amount of research is underway to help determine the risk factors, better ways to detect this condition and possible ways to prevent CTE in those with a history of concussion and head injury. From an article we published in February 2015 in the journal PLOS ONE, (Click Here to see Article) we found 150 autopsy confirmed cases of CTE in the world literature from 1954 to August 2013. (Three additional case were reported in the media) These cases are mostly divided between former boxers and former football players. The only common consistent finding thus far as a risk factor in the CTE case reports has been a history of prior brain trauma.
Because of these concerns an enormous amount of research is underway to help determine the risk factors, better ways to detect this condition and possible ways to prevent CTE in those with a history of concussion and head injury. From an article we published in February 2015 in the journal PLOS ONE, (Click Here to see Article) we found 150 autopsy confirmed cases of CTE in the world literature from 1954 to August 2013. (Three additional case were reported in the media) These cases are mostly divided between former boxers and former football players. The only common consistent finding thus far as a risk factor in the CTE case reports has been a history of prior brain trauma.
The CTE condition has been seen in a relatively few people and all were deceased. CTE is seen as a neurodegeneration brain cell problem and has been compared to Alzheimer’s disease where in similar changes of brain degeneration can be seen. It is well known that prior head injury is also a risk factor for the development of Alzheimer’s disease as well. But unlike CTE additional risk factors have been found with AD. These include: Advancing age, genetic mutations, family history of the disease and underlying heart and vascular disease. Whether these factors also play a role in the development of CTE is unknown at this time.
Common Symptoms Separately Reported in Alzheimer’s disease and CTE
- Memory problems
- Getting lost – Not recognizing surroundings
- Speech and Writing changes
- Difficulty with Reasoning Skills, Decision making and Judgment
- Personality changes
- Depression
- Social withdrawal
- Mood swings
- Distrust in others
- Irritability and aggressiveness
- Changes in sleeping habits
- Wandering
- Loss of inhibitions
- Delusions, such as believing something has been stolen
Inflammation and Brain Cell Health
What happens during mild brain trauma and concussion in the short-term is well known, but the long term consequences such as post-concussion and CTE are under intensive investigation. There is, however, a general agreement that brain cells are very sensitive to the environmental status of the brain. If blood oxygen levels are low we lose consciousness in one to two minutes and cell death can occur in seven. No other cells in the body are this fragile. This sensitivity is also true with low blood glucose levels, deficient levels of micronutrients, excessive stress hormones like cortisol and inflammatory factors such as free radicals.
Treatments to reduce inflammation to maintain brain health can be effective since inflammation in the brain has been linked to cognitive decline, neurodegeneration and metabolic abnormalities. The aging brain is also more prone to neuroinflammation. Inflammation throughout the body due to saturated dietary fats, smoking or other environmental toxins, stress, obesity or lack of exercise can contribute to poor brain health and premature brain aging.
Because there is no definitive medical treatment for CTE at this time, using Alzheimer’s disease as a treatment model of degenerative and inflammatory brain changes may help direct interventions that benefit those at risk for CTE.
What a New Harris Survey Says About a Disproportionate Fear of Concussion
 In October 2015 a survey sponsored by UPMC done by Harris Polling found that Americans are very concerned about concussions but are also poorly informed about concussion management and treatment. The survey results HERE, are some of the first ever done since sports concussion have been highlighted by the media.
In October 2015 a survey sponsored by UPMC done by Harris Polling found that Americans are very concerned about concussions but are also poorly informed about concussion management and treatment. The survey results HERE, are some of the first ever done since sports concussion have been highlighted by the media.
“This survey highlights the myths about concussion and the need for education. The reality is that we have made tremendous progress in the diagnosis, management and rehabilitation of this injury.” said Micky Collins, Ph.D., executive and clinical director of the UPMC Sports Medicine Concussion Program. “The study results are cause for concern because, given these advances, parents should not be living in fear. Sports can be an integral part in a child’s physical and social development. As clinicians and scientists, we need to disseminate more accurate information,” added Dr. Collins.
Dr Joseph Maroon is the Co-Director of the UPMC Sports Medicine Concussion Center, which is in one of the largest in the country.
“One of the more disturbing findings of the survey,” notes Dr. Maroon, “is the misunderstanding that concussion results in a life long condition that is untreatable. This is absolutely untrue and may be linked to media reportings and the biased sensationalism that surround this topic.”
- Barely 1 in 4 (29 percent) of Americans believe that all concussions can be treated
- 79 percent of adults incorrectly believe or are unsure that there is no real way to cure a concussion; the symptoms can only be lessened
- About 4 in 5 (81 percent) Americans aren’t comfortable that they would know the steps to manage or treat a concussion if they sustained one
Oct. 15-16, 2015 – UPMC Sports Medicine Concussion Program hosted one of the largest meeting of concussion experts with the purpose to develop best practice guidelines for concussion management. The meeting participants proposed standard guidelines on the best practices, protocols and active therapies for treating concussions today.
“The participants reached unanimous consent on the statement that concussions are treatable and rest after a concussion may not be for everyone”, per Dr Micky Collins, PhD. Nineteen other recommendations will be published in a white paper to be published in the medical journal Neurosurgery. Read more HERE
Improvements in NFL Player Concussion Prevention
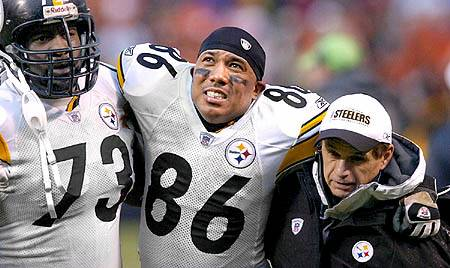
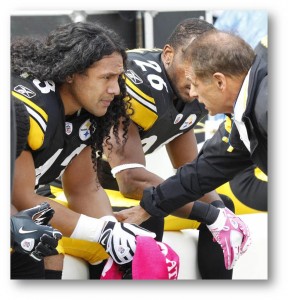 In September 2015 the Pittsburgh Post Gazette reported on just the latest change the NFL has enacted to reduce concussions and improve player concussion management. Reporter J. Brady McCollough wrote the article entitled, Eye in the Sky’ trainers monitor NFL players from high above action, where he discusses the new NFL concussion policy to require gameday observers to be placed in sky boxes to report on concussions that might not be seen by the sideline medical staff . This concept was trialed last year and is now is part of NFL safety and health policy for the players. As a trained medical profession, the observer can call a medical “time out” and require a player to be removed, at least for one play, so they can be evaluated by sideline medical personnel. As the Steelers team neurosurgeon Dr Maroon welcomes the idea. READ ARTICLE HERE
In September 2015 the Pittsburgh Post Gazette reported on just the latest change the NFL has enacted to reduce concussions and improve player concussion management. Reporter J. Brady McCollough wrote the article entitled, Eye in the Sky’ trainers monitor NFL players from high above action, where he discusses the new NFL concussion policy to require gameday observers to be placed in sky boxes to report on concussions that might not be seen by the sideline medical staff . This concept was trialed last year and is now is part of NFL safety and health policy for the players. As a trained medical profession, the observer can call a medical “time out” and require a player to be removed, at least for one play, so they can be evaluated by sideline medical personnel. As the Steelers team neurosurgeon Dr Maroon welcomes the idea. READ ARTICLE HERE
As the concussion issue became more prevalent in the public eye, team doctors began to be heard more easily. Dr. Yates, who served as president of the NFL Physicians Society, got to sit on the NFL’s competition committee. He believes good developments have happened with the help of about 25 rule changes geared toward lessening impacts to the head, and the numbers back him up.
The NFL states that, since 2012, concussions in regular season games are down 35 percent, and helmet-to-helmet hits are down 43 percent.
What can be Done to Improve Youth Sport Concussion Prevention?
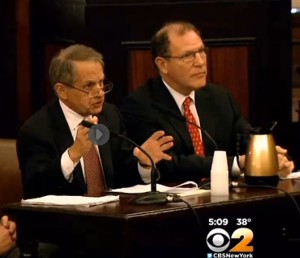 In January 2015 Dr Joseph Maroon presented expert testimony to the members of the NY City Council on a proposed rule on sideline medical coverage for organized youth football in the city. A new bill had been proposed by Council that would require placing doctors on the sidelines at youth games and practices to help prevent and treat concussions. Dr. Maroon supports new technology that would allow a virtual physician, through telemedicine, to attend the game in the event of a concussion. This could offer a solution to the enormous cost that would be required to hire a physician to actually be present at all youth football practices and games as has been proposed. See Website to CBS New York –HERE
In January 2015 Dr Joseph Maroon presented expert testimony to the members of the NY City Council on a proposed rule on sideline medical coverage for organized youth football in the city. A new bill had been proposed by Council that would require placing doctors on the sidelines at youth games and practices to help prevent and treat concussions. Dr. Maroon supports new technology that would allow a virtual physician, through telemedicine, to attend the game in the event of a concussion. This could offer a solution to the enormous cost that would be required to hire a physician to actually be present at all youth football practices and games as has been proposed. See Website to CBS New York –HERE
Dr. Joseph Maroon is a neurosurgeon for the Pittsburgh Steelers. He testified at the hearing in support of the bill, offering technology that would allow a virtual doctor on the sidelines. “You have an iPad where you can literally … the doctor can see the patient, can see the athlete and with a trainer, even a parent, examine and question and evaluate the patient,” Maroon said.
What are these New Technologies?
Recognizing the need for improved concussion prevention and management in youth sports several technology companies have developed new tools to help improve the safety of contact sports. These tools range from helmet sensors for measuring head impacts to sideline robots that are linked to physicians who can make critical concussion assessments at the moment of injury. The greatest need for these technologies are in youth contact sports, which generally lack medically trained sideline personnel. In the US there are about 3.5 million kids playing youth football. The proposed legislation in NYC and several communities, will mandate the same medical care be provided to youth football as available at the high school, college and professional levels.
The major technologies being developed include neurocognitive testing, sensors, for recording the location, number and magnitude of head hits and systems to provide a virtual physician presence at all games and contact practices. ImPACT Technologies®, is a leader in the area of neuropsychological testing and is now focused on developing baseline testing for children as young as 5 years old. If a concussion were to occur the baseline test can be used to compare to a new test in order to assist in return to play decisions. Several head impact sensor system are currently being trialed at major universities across the US. They can detect the number, location and magnitude of head impacts and store the information for ongoing dosimetry-like purposes. Telemedicine system, which has been available for rural communities is being upgaraded to provide a virtual physician trained in concussion management to be available at any youth football game or practice in the country when needed for concussion evaluation and treatment recommendations.
All three of these technological innovations are being assessed individually and as a part of a unified program. A network of these new technologies will soon be available to provide a new safety model for youth participating in contact sports and in particular, football. This approach has the opportunity to be cost effective and also more comprehensive since a history of prior hits to the head and concussions can in stored within the network and assessed as needed.
What are Concussions: In a nutshell
A concussion, also called “mild Traumatic Brain Injury” (mTBI), describes an injury to the brain resulting from a forceful impact to the head that results in transient neurological symptoms. This trauma to the brain causes electrical and metabolic changes that can cause headaches, dizziness, fogginess and others. Concussion symptoms include changes in mental status, such as confusion or memory loss and may include other symptoms such as sleep problems, nausea, trouble concentrating or irritability (see table).
What causes a Concussion?
Any injury that causes the brain to suddenly and rapidly move may cause a concussion. Typical circumstances are a sudden, forceful impact to the head, such as a blow to the head or crashing the head into something (or someone). Violent shaking of the head can also lead to a concussion. Common settings for concussions to occur are falls, impact sports such as football or boxing, military duties with exposure to explosions or (car) accidents.
What are symptoms of a Concussion?
The most typical symptoms involve alteration of mental status, such as confusion and amnesia (memory loss) about the event itself and/ or a time period before the event (e.g. the beginning of the game). Loss of consciousness typically doesn’t occur except in the most severe cases of concussions (about 10%).
After the impact, symptoms include one or more of the following to meet criteria of a concussion: Headaches, blurred vision, altered balance, nausea & vomiting, dizziness, fatigue, sleep disturbances, change in sense of smell and/or taste, mood swings, anxiety, apathy, irritability, poor memory, confusion, poor attention and inability to focus.
What is Post -Concussion Syndrome?
Although the majority of people who experience a concussion are likely to recover, some individuals may experience chronic cognitive and neurobehavioral difficulties related to recurrent injury. Such symptoms may include chronic headaches, fatigue, sleep difficulties, personality change (e.g. increased irritability, emotionality), sensitivity to light/noise, dizziness when standing quickly, and deficits in short-term memory, problem solving and general academic functioning. This constellation of symptoms is referred to “Post-Concussion Syndrome” and can be quite disabling for an athlete. In some cases, such difficulties can be permanent and disabling.
What are the Risks of Not Treating a Concussion?
In addition to Post-Concussion Syndrome, suffering a second blow to the head while recovering from an initial concussion can have catastrophic consequences as in the case of “Second Impact Syndrome,” which has led to approximately 30-40 deaths in mostly athletes over the past decade. If not fully recovered from an initial concussion the brain is significantly vulnerable for recurrent, cumulative, and even catastrophic consequences of a second concussive injury. To try and reduce the risk of post concussion syndrome and second-impact syndrome after a concussion the person will need time to recover from concussion. This may take days to weeks to months to recover and therefore a healthcare profession should be consulted to manage your care and return to play decisions for athletes. No athlete should return to sport or other at-risk participation when symptoms of concussion are present and recovery is ongoing. In summary, the best way to prevent difficulties with concussion is to manage the injury properly when it does occur.
How are Concussions Treated?
Traditional neurological and radiological procedures, such as CT, MRI, and EEG, although helpful in identifying more serious head injuries (e.g. skull fracture, hematoma, contusion), are not useful in identifying the effects of concussion. Such tests are typically normal, even in athletes sustaining a severe concussion. Managing a concussion should be individualized and comprehensive medical management of concussion is optimal. Modern concussion management in athletes utilizes baseline and/or post-injury neurocognitive testing. Such evaluation can help to objectively evaluate the concussed athlete’s post-injury condition and track recovery for safe return to play, thus helping to prevent the cumulative effects of concussion.
Neurocognitive testing is the “cornerstone” of proper concussion management, along with physician evaluation to determine return to play activity. ImPACT™ is a user-friendly computer based testing program specifically designed for the management of sports-related concussion. The instrument has been designed after approximately 10-years of University-based, grant-supported research. ImPACT™ is currently the most widely utilized computerized program in the world and is implemented effectively across high school, collegiate, and professional levels of sport participation.
In some case prolonged symptoms of of concussion can occur. This is known as post-concussion syndrome (PCS). UPMC’s Sports Medicine Concussion Program, is one of the country’s leading programs on managing and treating PCS. We known now that concussion symptoms are s treatable. Treatment may include active rehab, active physical therapies and other approaches. The concept of active treatment and in many cases avoiding strict rest after every concussion is now being advocated by many who specialize in concussion injury. The hope of active treatment for PCS management is to help reduce long-term effects. The UPMC’s concussion program has identified six subtypes of concussion, including: cognitive/fatigue; vestibular, which affects balance; ocular, which involves vision; post-traumatic migraine; cervical, affecting the neck and spinal cord; and anxiety/mood. People may experience combinations of symptoms, but they can usually be organized and ranked using the subtypes. Various treatment specifics are used for each of these subtypes. Examples may include vision exercises or physical exercise for people with concussion-related anxiety.
I heard the term “subconcussive blow to the head”. What does that mean?
Impact to the head can vary in intensity. On one end of the spectrum are very mild impacts to the head (e.g. mildly hitting your head against a door), which may hurt and leave a bruise, but the protective system of the skull, membranes and CSF is able to avoid any impact on the brain, i.e. no brain damage occurs. On the opposite end, one high-intensity impact to the head will exceed the coping ability of the protective mechanism and will lead to a concussion, as discussed above.
However, there are blows to the head that have a moderate intensity, somewhere between mild and high-intensity: these impacts will exceed the brains protective mechanism’s ability to cope slightly, and the brain will suffer slight damage. However, the damage is not severe enough to cause any symptoms, and it will most likely heal fast and go unnoticed. Such an impact would be described as a subconcussive blow to the head.
This type of impact is important to understand when thinking about concussion prevention. An athlete who suffered a subconcussive blow to the head does not experience any symptoms, despite possibly having slight brain damage. If this athlete does not get enough time for the brain to fully heal before another impact to the head occurs, an accumulation of slight damages may occur and eventually a comparatively low-intensity impact to the head may result in brain trauma that qualifies as a concussion.
Tri-State Neurosurgical Associates-UPMC
Administrative Oakland Office Address:
Presbyterian University Hospital
Department of Neurosurgery
Suite 5C
200 Lothrop Street
Pittsburgh, PA 15213
Phone: 1-888-234-4357
© 2013 Tri-State Neurosurgical Associates – UPMC


 Dr. Maroon received an athletic scholarship to Indiana University in Bloomington, Indiana where as an undergraduate, he was named a Scholastic All-American in football. Dr. Maroon has successfully maintained his personal athletic interests through participation in 9 marathons and more than 72 Olympic-distance triathlon events. However, his greatest athletic accomplishment is his participation in 8 Ironman triathlons (Hawaii – 1993, 2003, 2008, 2010, 2013; Canada – 1995; New Zealand – 1997; Germany – 2000), where he usually finishes in the top 10 of his age group. Recently, in July 2012 and 2013, he finished second and third, respectively, in his age group in the Muncie, Indiana half Ironman triathlon. In October 2013 he completed his 5th World Championship Ironman in Kona, Hawaii.
Dr. Maroon received an athletic scholarship to Indiana University in Bloomington, Indiana where as an undergraduate, he was named a Scholastic All-American in football. Dr. Maroon has successfully maintained his personal athletic interests through participation in 9 marathons and more than 72 Olympic-distance triathlon events. However, his greatest athletic accomplishment is his participation in 8 Ironman triathlons (Hawaii – 1993, 2003, 2008, 2010, 2013; Canada – 1995; New Zealand – 1997; Germany – 2000), where he usually finishes in the top 10 of his age group. Recently, in July 2012 and 2013, he finished second and third, respectively, in his age group in the Muncie, Indiana half Ironman triathlon. In October 2013 he completed his 5th World Championship Ironman in Kona, Hawaii.