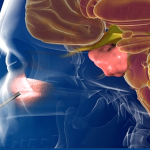
Endoscopic Endonasal Approach for pituitary tumors
 Summary:
Summary:- EEA is a minimally invasive method to approach pituitary tumors through the nasal cavities.
- EEA allows to access areas of the brain that were previously inoperable.
 A new method of performing pituitary surgery: the Endoscopic Endonasal Approach (EEA)
A new method of performing pituitary surgery: the Endoscopic Endonasal Approach (EEA)
In the past, pituitary lesions often were inoperable, and if surgery was possible, they used to be addressed through traditional open skull surgery. The EEA is an innovative minimally invasive procedure that uses the nose and nasal cavities to access the skull base. This approach is ideal for tumors located in or near the pituitary gland. EEA enables surgeons to treat conditions in critical areas of the brain, skull base, and upper spine that were once considered to be inoperable or hard to reach.
Summary of Benefits of of EEA instead of traditional open craniotomies
The Endoscopic Endonasal Approach (EEA) is an innovative minimally invasive procedure that uses the nose and nasal cavities to access the skull base. This approach is ideal for tumors located in or near the pituitary gland. EEA enables surgeons to treat conditions in critical areas of the brain, skull base, and upper spine that were once considered to be inoperable or hard to reach.
No incisions to heal
- EEA does not involve incisions or disfigurement to the patient’s skull or face.
- Patients with malignant tumors can start chemotherapy or radiation treatment almost immediately, without needing to wait for incisions to heal. This gives complementary therapies the chance to start working sooner.
Faster recovery time
- Recovery time from EEA can be days instead of the weeks or months of recovery that typically come with traditional open surgery.
- Patients often can be discharged from the hospital within one or two days.
Fewer side effects
- There are fewer, if any, lingering side effects than with traditional craniofacial surgery.
Reduced risk of neurological damage
- The brain does not have to be manipulated with EEA, reducing the likelihood of damage.
- Surgeons are better able to preserve important nerves that control vision and hearing.
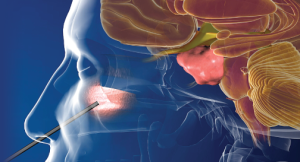
The Endonasal Endoscopic Approaches to Pituitary Tumor – more details
The use of a minimally invasive endoscope had been used extensively in gynecology, laparoscopy (abdominal surgery), thoracic (chest), and cardiac surgery. This endoscopic technique of visualization functions on the principle of a flashlight rather than a cone of light. The microscope starts of as wide base that then focuses light to a narrow point creating a cone of light. This requires a wide exposure to deliver a small area of visualization ‘cone of light.’ In comparison, the endoscope starts of as a narrow light source that then widens to provide a ‘flashlight’ view.
In 1999 the skull base program at UPMC made a formal commitment to take advantage of this technology for accessing the skull base. Believing that if we could create a conduit that was narrow to go through the face, we could deliver the flashlight to access the base of the skull and then progressively the brain. The nose provided the ideal conduit. While much work had already been done in the Ear-Nose-and Throat field in using the nose to access the region, it had stopped short of accessing the skull base. We extended this knowledge and procedure in order to approach and take out lesions of the skull base and of the brain itself. This approach allows one to work from ‘inside out,’ i.e. start directly at the target and work outward. In the process it would not require the layers of facial skeletal removal that were common with conventional approaches. In fact, there is no need for incisions at all as the nose provides the passage.
UPMC is now recognized as a Center of Excellence for the development of this technology. The Endonasal Endoscopic Approach allows extended access to pituitary tumors and makes it possible to remove them completely through the nostril. This type of tumor approach allows surgeons to more easily deal with the many fine structures around the pituitary gland, such as critical nerves and arteries. EEA minimizes the manipulation to these fragile structures, which minimizes the risk of negatively affecting them.
In essence, the EEA procedure allows the resection of the tumor to be done with minimal disturbance to the surrounding tissues. We no longer need to make incisions and disassemble the face so we can deliver a “cone of light” (microscope) to the skull base. Instead we can now deliver a ‘flashlight’ (endoscope/telescope) directly to the target via the nostril. This has the potential to reduce the impact on the patient, lessen the morbidity, and reduce the length of stay in many cases. Some procedures are now performed as overnight stays, with the patient, in some instances, returning to work in days.
Why come to Dr. Maroon at UPMC?
UPMC is a national leader and referral center for the evaluation and treatment of pituitary tumors, pituitary adenomas, and tumors or disorders of the hypothalamic-pituitary region. Dr. Maroon works with highly regarded specialists of the Departments of Neurosurgery, Endocrinology, Ear-Nose-and Throat, Radiology, Radiation Therapy and Neuro-Ophthalmology at UPMC to evaluate and treat patients with pituitary tumors and disorders. The specialists who make up this multidisciplinary program are leaders in their respective fields and have combined to make UPMC one of the most comprehensive programs in the country.


 Dr. Maroon received an athletic scholarship to Indiana University in Bloomington, Indiana where as an undergraduate, he was named a Scholastic All-American in football. Dr. Maroon has successfully maintained his personal athletic interests through participation in 9 marathons and more than 72 Olympic-distance triathlon events. However, his greatest athletic accomplishment is his participation in 8 Ironman triathlons (Hawaii – 1993, 2003, 2008, 2010, 2013; Canada – 1995; New Zealand – 1997; Germany – 2000), where he usually finishes in the top 10 of his age group. Recently, in July 2012 and 2013, he finished second and third, respectively, in his age group in the Muncie, Indiana half Ironman triathlon. In October 2013 he completed his 5th World Championship Ironman in Kona, Hawaii.
Dr. Maroon received an athletic scholarship to Indiana University in Bloomington, Indiana where as an undergraduate, he was named a Scholastic All-American in football. Dr. Maroon has successfully maintained his personal athletic interests through participation in 9 marathons and more than 72 Olympic-distance triathlon events. However, his greatest athletic accomplishment is his participation in 8 Ironman triathlons (Hawaii – 1993, 2003, 2008, 2010, 2013; Canada – 1995; New Zealand – 1997; Germany – 2000), where he usually finishes in the top 10 of his age group. Recently, in July 2012 and 2013, he finished second and third, respectively, in his age group in the Muncie, Indiana half Ironman triathlon. In October 2013 he completed his 5th World Championship Ironman in Kona, Hawaii.