Lumbar Spinal Fusion Without Metal Rods and Screws
 Summary:
Summary:- Advancements in spine surgery have allowed some patients who need lumbar fusion to avoid metal rods and pedicle screws
- Faster recovery
- Typically discharged is one day after surgery
Introduction
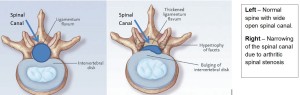
A Lumbar Laminectomy is a surgical procedure designed to decompress and relieved spinal cord and nerve compression in the lower back due to a condition called spinal stenosis. Spinal stenosis is a degenerative arthritic condition that occurs over time and slowly compresses the spinal canal, which contains the spinal cord and nerve roots that exit to the legs. When the canal narrows, it pinches the nerves, which results in lower back pain and often numbness, weakness and pain in the legs. Symptoms are often made worse with walking. In severe cases, the bladder and bowel may also be affected.
(Click on Images to see full size)
Spinal Stenosis is often associated with collapse of the disc spaces between the vertebrae, a condition called spondylosis. In this condition, greater pressure is being put on the joints between the vertebrae. These joints, called facet joints, can begin to enlarge and become unstable requiring additional fusion surgery in some cases. If the facet joints and spinal stenosis progresses, a condition called “spondylolisthesis” can develop. This condition exists when there is slippage of one vertebral body over another, and the result is pain associated with nerve compression. The varying degree of slippage may cause further spinal instability that requires a fusion operation to be done at the same time that stenosis is surgically addressed. In summary, the lumbar laminectomy is intended to decompress the area of stenosis and, if required, the fusion is performed to prevent any movement that can destabilize the spinal segments.
What Surgery is Needed?
The surgery used to treat nerve compression due to spinal stenosis is called “laminectomy”. Depending on the levels of the spine requiring decompression, an incision is made in the lumbar area, and the lamina, or outer bone of the vertebra, is exposed. With the use of specialized instruments and an operating microscope, the lamina is removed along with any other compressive tissues. The nerve roots that connect to the legs are then decompressed and the pressure is relieved. If the spine has degenerated to the extend that the facet joints have become unstable and move slightly (spondylolisthesis), Dr. Maroon may recommend a spine fusion in addition to the laminectomy to release the pressure from the nerves and stabilize the spine.
TruFUSE™ Facet Fusion – No Screws Required
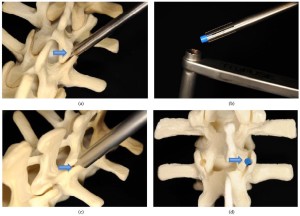
Recent advancements in spine surgery have allowed some patients who need lumbar fusion to avoid metal rods and pedicle screws being placed in their spine following a laminectomy. If Dr. Maroon has recommended a lumbar fusion, he now typically uses a facet fusion system called TruFUSE™. TruFUSE™ is a small cylinder (depicted below in blue) of bone that is inserted into the unstable facet joint in order to lock it in place. It is placed in both the right and left facet joints and usually additional bone is placed alongside it to enhance the fusion process. Most people will be asked to wear a brace after surgery for 4-8 weeks until the bone fusion is strong enough to make a brace unnecessary.
Recovery following TruFUSE ™ Facet Fusion
In general, the laminectomy surgery lasts 1 to 2 hours and typically the placement of the TruFUSE™ bone does not add significant time to the surgery. Most patients can be sent home the day after surgery and will be asked to wear a brace when not in bed. Prior to your return appointment about one month after surgery, you will be asked to obtain an x-ray of your spine in order to determine how well the surgery site is healing. Back and incisional pain is common after surgery but generally tolerable with pain medications. Additional instructions will be provided to you at the time of your discharge from the hospital.
What are the Advantages of TruFUSE™ over Screws and Rods for Fusion?
Because every person is different and their surgical needs are different, the type of surgery selected must fit the individual. The use of TruFUSE™ will be matched with the individual, based on its benefits and limitations, and the use of TruFUSE ™ or traditional rod and pedicle screw fusion will be determined by Dr Maroon based on a variety of neurosurgical criteria. But there are advantages to having a TruFUSE™ fusion in those patients who in the past may have only been offered rod and pedicle screw fusions.
In 2013 Dr. Maroon evaluated over 40 of his patients who had required a laminectomy and fusion with the TruFUSE™ facet fusion. This research was published and below is a summary of the findings along with advantages that were found when comparing his results to studies that used pedicle screw and rod fusion systems.
Facts and Advantages of TruFUSE™ over Traditional Fusion
- No evidence of post–operative facet fracture or TruFUSE™ bone dowel dislodgement on any post-operative x-rays including flexion and extension
- 80% of patients reported improvement, ranging from somewhat to excellent, compared to pre-operative statements
- Total operative time 1 hr. and 40 minutes on average
- On average about 5 oz. blood loss – no transfusions needed
- Average hospital stay was about 1.7 days
Of course, no two patients will experience the same results. This information is merely intended to help you better understand the underlying problem and the surgery options. Dr. Maroon and his team will always explain specific circumstances as they apply to your individual case.
Tri-State Neurosurgical Associates-UPMC
Administrative Oakland Office Address:
Presbyterian University Hospital
Department of Neurosurgery
Suite 5C
200 Lothrop Street
Pittsburgh, PA 15213
Phone: 1-888-234-4357
© 2013 Tri-State Neurosurgical Associates – UPMC


 Dr. Maroon received an athletic scholarship to Indiana University in Bloomington, Indiana where as an undergraduate, he was named a Scholastic All-American in football. Dr. Maroon has successfully maintained his personal athletic interests through participation in 9 marathons and more than 72 Olympic-distance triathlon events. However, his greatest athletic accomplishment is his participation in 8 Ironman triathlons (Hawaii – 1993, 2003, 2008, 2010, 2013; Canada – 1995; New Zealand – 1997; Germany – 2000), where he usually finishes in the top 10 of his age group. Recently, in July 2012 and 2013, he finished second and third, respectively, in his age group in the Muncie, Indiana half Ironman triathlon. In October 2013 he completed his 5th World Championship Ironman in Kona, Hawaii.
Dr. Maroon received an athletic scholarship to Indiana University in Bloomington, Indiana where as an undergraduate, he was named a Scholastic All-American in football. Dr. Maroon has successfully maintained his personal athletic interests through participation in 9 marathons and more than 72 Olympic-distance triathlon events. However, his greatest athletic accomplishment is his participation in 8 Ironman triathlons (Hawaii – 1993, 2003, 2008, 2010, 2013; Canada – 1995; New Zealand – 1997; Germany – 2000), where he usually finishes in the top 10 of his age group. Recently, in July 2012 and 2013, he finished second and third, respectively, in his age group in the Muncie, Indiana half Ironman triathlon. In October 2013 he completed his 5th World Championship Ironman in Kona, Hawaii.