Introduction
When an athlete, whether it is football, soccer, lacrosse or any sport, suffers a blow to head depending on the force, direction and condition of the athlete a concussion can occur. It can be painful for the athlete as well as frightening to a spectator to watch. We instinctively know we must protect our brain from trauma. Our hands reflexively move to our head to block an incoming blow.
Over the last several years concussion researchers and the medical community have reported definitive evidence that a brain concussion may have both short-term and long-term negative consequences and must be treated properly just like any other injury. Despite this isolated media stories continue report on athletes from pee-wee leagues through the pros who are still ignoring these warning and lying about having suffered a concussion.
Research being done on those that suffered a concussion, both living and deceased, continues to suggest that blows to the head can have consequences to both brain function and structure. Like all other organs and parts of the body the consequences of abuse will eventually be revealed as we age. A knee joint traumatized daily in sport with running, stopping, twisting and being hit will eventually develop stiffness, soreness, swelling and degenerative changes leading to some type of disability. The brain may also suffer in this same way as a result of trauma and just as with the knee the mechanism is most likely in part due to our own body’s inflammatory response. Prevention and proper initial management are essential.
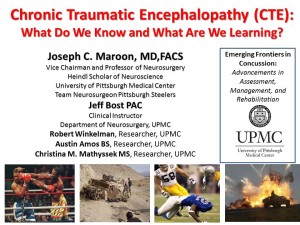
Chronic progressive traumatic encephalopathy or CTE
Since the late 1920’s scientist have recognized head trauma can induce neurodegeneration when examined during an autopsy. First described as “Punch drunk syndrome” in boxers, later called dementia pugilistica (DP), and then more recently chronic progressive traumatic encephalopathy or CTE this condition has become a major health concern in amateur and professional sports. Currently, there are no definitive tests to distinguish CTE from other neurodegenerative diseases other than by evaluation of brain tissue. For this reason published reports of CTE thus far have been limited to individual and small collections of case studies of mostly former athletes who had a history of dementia or major psychological issues.
CTE has now been reported in a wide range of individual athletes, combat military personnel and others who had suffered some form of traumatic brain injury (TBI) years to decades prior to their deaths. Because concussions and blows to the head are common in both sports and the military there is a concern by many former athletes and veterans that symptoms of dementia and other brain related problems, especially with aging, may have some relationship to prior head trauma.
From an article published in February 2015 in the journal PLOS ONE, (Click Here to see Article) we found 150 autopsy confirmed cases of CTE in the world literature from 1954 to August 2013. (Three additional case were reported in the media) These cases are mostly divided between former boxers and former football players. The only common consistent finding thus far as a risk factor in the CTE case reports has been a history of prior brain trauma.
Brain Degeneration: CTE vs Alzheimer’s Disease
Because of these concerns an enormous amount of research is underway to help determine the risk factors, better ways to detect this condition and possible ways to prevent CTE in those with a history of concussion and head injury. At the current time there have been approximately only 150 autopsy confirmed cases of CTE. These cases are mostly divided between former boxers and former football players. The only common consistent finding thus far for as a risk factor in the CTE case reports has been a history of prior brain trauma.
Because CTE condition has been seen in a relatively small number deceased people and all other research models are being used to understand CTE. Alzheimer’s disease (AD) is considered a comparable model due to similar changes seen in brain degeneration (called neurodegeneration) and the similar neurological decline as often found with CTE. Prior head injury is also a risk factor for the development of AD as well. But unlike CTE additional risk factors have been found with AD. These include: Advancing age, genetic mutations, family history of the disease and underlying heart and vascular disease. Whether these factors also play a role in the development of CTE is unknown at this time.
AD has now been studied for decades and much is known about what happens to brain cells as AD degenerative changes start to occur in the brain. AD in the past was generally believed to progress no matter what treatments or interventions were tried to slow or stop the condition. There are now recent advances both in pharmaceuticals and nutritional treatments along with behavioral and lifestyle changes which have proven very beneficial to slow AD symptoms and brain cell changes. Specifically, large population studies investigating AD report lifestyle, habits, diet, nutritional status, types of medications and dietary supplements allow certain people to be less likely to suffer from AD. One of the reoccurring findings in these studies has indicated that those interventions that can reduce brain inflammation and improve optimal nutritional supplies to the brain put people at less risk for developing AD.
Lifestyle Factors Often Associated with Alzheimer’s disease:
- Lack of exercise
- Smoking
- High blood pressure
- High blood cholesterol
- Poorly controlled diabetes
- A diet lacking in fruits and vegetables
- Lack of social engagement
Common Symptoms Reported/Seen in those with Alzheimer’s disease and CTE
- Memory problems
- Getting lost – Not recognizing surroundings
- Speech and Writing changes
- Difficulty with Reasoning Skills, Decision making and Judgment
- Personality changes
- Depression
- Social withdrawal
- Mood swings
- Distrust in others
- Irritability and aggressiveness
- Changes in sleeping habits
- Wandering
- Loss of inhibitions
- Delusions, such as believing something has been stolen
Inflammation and Brain Cell Health
What happens during mild brain trauma and concussion in the short-term is well known, but the long term consequences such as post-concussion and CTE under intensive investigation. There is, however, a general agreement that brain cells are very sensitive to the environmental status of the brain. If blood oxygen levels are low we lose consciousness in one to two minutes and cell death can occur in seven. No other cells in the body are this fragile. This sensitivity is also true with low blood glucose levels, deficient levels of micronutrients, excessive stress hormones like cortisol and inflammatory factors such as free radicals.
Treatments to reduce inflammation to maintain brain health can be effective since inflammation in the brain has been linked to cognitive decline, neurodegeneration and metabolic abnormalities. The aging brain is also more prone to neuroinflammation. Inflammation throughout the body due to high dietary fats, smoking or other environmental toxins, stress, obesity or lack of exercise can contribute to poor brain health and premature brain aging.
Because there is no definitive medical treatment for CTE at this time using AD as a treatment model of degenerative and inflammatory brain changes may help direct interventions that benefit those at risk for CTE.
Below are several healthy interventions known to both strengthen and weaken brain cells and inflammation in both the body and brain.
Dietary Interventions to Inflammation
Dietary components such as diets rich in saturated fats, transfats (hydrogenated or partially hydrogenated oils), and processed foods with lots of simple sugars can stimulate inflammation. Diets such as the Mediterranean diet rich in olive oil, fruits and vegetables, nuts, beans, and whole grains has been shown to reduce inflammation. Consuming alcohol only in moderation has been associated with less inflammation compared to excessive alcohol intake can increase inflammation. In general one to two glasses of red wine per day can also provide the benefit of concentrated polyphenols, which are known to have antioxidant properties, have been found to provide a health benefit.
The essential fatty acids omega-3 found in oily fish and fish oil supplements contain molecules known to decrease several markers of inflammation, whereas increasing dietary intake of omega-6 fatty acids found in corn oils and most processed foods can increases inflammatory markers. Other supplements such as vitamins, minerals, and herbs can reduce inflammation levels. Spices turmeric (curcumin), ginger and Boswellia serrate can inhibit inflammatory pathways. Catechins, found in teas, have antioxidant and anti-inflammatory effects. Alpha-lipoic acid, as a dietary supplement, has anti-inflammatory properties.
Lifestyle Interventions to Inflammation
Maintaining a healthy body weight has been shown to control chronic inflammatory diseases and also weight loss has been shown to decrease chronic disease such as diabetes and even cognitive decline and AD. Smoking cessation and reduced exposure to environmental pollution has been reported to decrease all biomarkers of inflammation. Stress results in the release of a hormone called cortisol the can actually kill brain cells if the stress remains chronic. Stress reduction can not only help to preserve brain cells it can lower blood pressure and risk for heart disease and stroke.
Regular physical exercise is good for us, no matter what our age. This is especially true as we age. Exercise supports a healthy heart and blood pressure, healthy immune system and improved blood sugar levels. Recent research shows that regular physical exercise can also improve brain function and reduce memory problems associated with aging. Physical exercise has a major strengthening impact on the structure of the brain. Both animal and human cell studies have shown that exercise causes new nerve cells to grow, called neurogenesis, disproving a once held belief that humans can’t grow new brain cells. Exercise can cause the release of BDNF, a hormone, which has the capacity to increase the number of brain cells and their connections which can potentially improve memory and learning.
REF:
Maintaining Brain Health by Monitoring Inflammatory Processes: a Mechanism to Promote Successful Aging, Maintaining Brain Health by Monitoring Inflammatory Processes: a Mechanism to Promote Successful Aging Aging and Disease. 2012 February; 3(1)16
Acheson A, Conover JC, Fandl JP, DeChiara TM, Russell M, Thadani A, Squinto SP, Yancopoulos GD, Lindsay RM (March 1995). A BDNF autocrine loop in adult sensory neurons prevents cell death. Nature 374 (6521): 450–3.
Colcombe SJ, Erickson KI, Scalf PE, et al. Aerobic exercise training increases brain volume in aging humans. Gerontol A Biol Sci Med Sci 2006;61(11):1166-1170.
Ferris LT, Williams JS, Shen CL. The effect of acute exercise on serum brain-derived neurotrophic factor levels and cognition function. Med Sci Sports Exerc 2007;39(4):728-734.
Yaffe K, Barnes D, Nevit M, et al. A prospective study of physical activity and cognitive decline in elderly women. Arch Intern Med 2001;161:1703-1708.
Laurin D et al. 2001 Physical activity and risk of cognitive impairment and dementia in elderly persons. Arch Neurol 58;498-504.
Maroon, JC, The Longevity Factor: How Resveratrol and Red Wine Activate Genes for a longer and Healthier Life, Simon and Schuster 2009.
Tri-State Neurosurgical Associates-UPMC
Administrative Oakland Office Address:
Presbyterian University Hospital
Department of Neurosurgery
Suite 5C
200 Lothrop Street
Pittsburgh, PA 15213
Phone: 1-888-234-4357
© 2015 Tri-State Neurosurgical Associates – UPMC


 Dr. Maroon received an athletic scholarship to Indiana University in Bloomington, Indiana where as an undergraduate, he was named a Scholastic All-American in football. Dr. Maroon has successfully maintained his personal athletic interests through participation in 9 marathons and more than 72 Olympic-distance triathlon events. However, his greatest athletic accomplishment is his participation in 8 Ironman triathlons (Hawaii – 1993, 2003, 2008, 2010, 2013; Canada – 1995; New Zealand – 1997; Germany – 2000), where he usually finishes in the top 10 of his age group. Recently, in July 2012 and 2013, he finished second and third, respectively, in his age group in the Muncie, Indiana half Ironman triathlon. In October 2013 he completed his 5th World Championship Ironman in Kona, Hawaii.
Dr. Maroon received an athletic scholarship to Indiana University in Bloomington, Indiana where as an undergraduate, he was named a Scholastic All-American in football. Dr. Maroon has successfully maintained his personal athletic interests through participation in 9 marathons and more than 72 Olympic-distance triathlon events. However, his greatest athletic accomplishment is his participation in 8 Ironman triathlons (Hawaii – 1993, 2003, 2008, 2010, 2013; Canada – 1995; New Zealand – 1997; Germany – 2000), where he usually finishes in the top 10 of his age group. Recently, in July 2012 and 2013, he finished second and third, respectively, in his age group in the Muncie, Indiana half Ironman triathlon. In October 2013 he completed his 5th World Championship Ironman in Kona, Hawaii.